Epidemiological data from all over the world has shown a global struggle with pain , specifically – lower back pain.
The United Nations and World Health Organization has recognized chronic pain as a global burden in need of significant attention.
The data suggests that 56 percent of people globally suffer from regular body pain on a weekly basis.1
We know the world is in pain and many of us, if not all of us, have experienced some sort of pain in our lifetimes that would be considered chronic.
It is an understatement that we need a way to fix lower back pain.
This article will be split into two sections.
In the first section, we will do a deep dive on pain biology and pain history.
The second section will be how all of that information relates to lower back pain.
By first understanding how pain works, you can then apply it to your unique pain situation and ultimately relieve the pain you are experiencing.
Educating my clients about pain and helping them to understand their pain has been a key component to finding relief from their pain.
How I Cured My Lower Back Pain
Before we begin, I wanted to quickly share a personal story about my back pain struggles and how I fixed my lower back pain.
In college I began lifting heavy weights with improper form and soon developed recurring back pain that eventually turned chronic.
I initially went to doctors for answers but left disappointed as I soon realized that they did not provide me with any solution to my pain.
I eventually began working with an amazing physical therapist who was able to treat my back pain once and for all.
After I successfully treated my pain, I was so inspired that I wanted to help my clients find a solution to their pain.
I had been heavily focused on strength training and the majority of my clients were athletes.
I soon realized it was much more rewarding to help people regain function and get out of pain and so I focused on helping these individuals almost exclusively.
The majority of my clients now are looking to move in a functional, pain-free way and I believe the strategies that I will teach you in this article are the foundational principles that will allow you to relieve your lower back pain.
As you will read later on, the foundational exercises that solved my back pain and many others can be found with video explanations in this free guide and also this article.
But more on that later – let’s start by laying the foundation and understanding what pain really is.
What is Pain and What is Chronic Pain?
But what is pain and what is chronic pain?
This is a central question to answer if we are to learn how to fix lower back pain.
Well the latter is a bit easier to define.
Chronic pain can be defined as pain that persists beyond normal tissue healing time which is generally thought to be between three and six months.2
Broadly speaking, pain cannot be defined by a strict physiological definition.
Nor can pain be boiled down to a unanimous phenomenon that all organisms experience in the same way, both interspecies specific and intraspecies specific.
I would like to take a moment to formally thank the International Pain and Spine Institute, Adriaan Louw and all colleagues for the beautiful images that you will see throughout my article. They are not my designs and the infographics serve as great tools for teaching pain science.
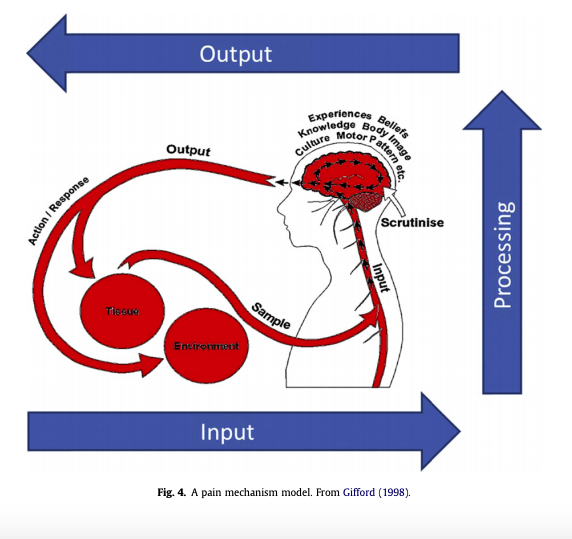
(Infographic Courtesy of Gifford (1998))
The History of Pain
If we are to consider our species, Homo Sapiens – the experience of pain is one so complex that we have hardly figured it out, despite many recent advances in medical science.
However, the Cartesian model of pain has largely persisted in our current medical model and has led many to feel hopeless amongst its shortcomings.
Rene Descartes was a French Philosopher, mathematician and scientist who was considered to be the father of modern western philosophy.
In his 1644 Treatise of Man, he theorized that the body was like a machine and that pain was a disturbance passed down along nerve fibers until the disturbance reached the brain.
Should I Be Worried About My Pain?
In a broad sense, the current medical model has continued to employ this ideology as a central tenant to the conceptualization of pain.
Subsequently, they have anchored the public understanding of pain.3
The current medical model has led people to catastrophize and worry about their lower back pain.
Such assumptions include the following:
1.) There is a direct link between the amount of tissue damage and the level of pain experienced.
2.) All pain is caused by injury and increased pain means more damage.
3.) Pain is either physical or psychological.
4.) In chronic pain, the tissue is not healing and so pain goes on.
5.) Nervous system function is simplistic like a wire.
With these assumptions come a great deal of fear and worry about pain.
So many people catastrophize about their pain because of a diagnosis given to them by a ‘medical professional.’
The truth is, you don’t need to be worried.
Your body has an incredible capability to heal and your first step is to have faith!
You can fix your lower back pain!
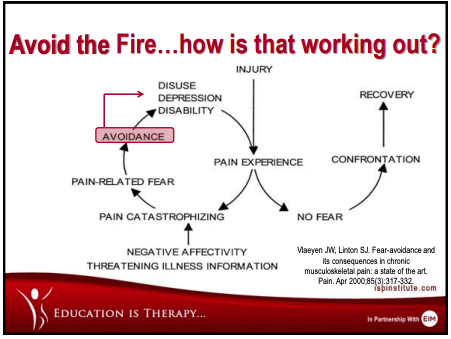
(Infographic Courtesy of the International Pain and Spine Institute)
How the Current Medical Model Treats Pain
The current medical model has suggested that every disease process can be explained in terms of an underlying deviation from normal function.
The model implies that pathology and symptoms are correlated such that a greater expression of symptoms would indicate greater underlying pathology.
The proposed correction of such biomechanical insufficiencies such as surgery, injections, manipulation or exercise is supposed to eliminate the symptoms and restore the patient to normal functioning.
Why is it then that so many patients who demonstrate diagnostic signs of recovery continue to report symptoms and pain?
Surely if the biomechanical dysfunction has been addressed and the tissue repaired, then the pain should subside right?
Well it turns out not to be this simple.
The experience of pain is a multifaceted process intertwined with the biopsychosocial network at the core of its underpinnings.
Pain is not simply physiological.
It is a psychological experience. It is a social experience. It is an amorphic experience largely subjective to the individual facing it.
Does Pain Mean Dysfunctional?
It has been well documented that many asymptomatic, ‘healthy’ individuals – have diagnostic evidence of pathology yet experience no pain at all.
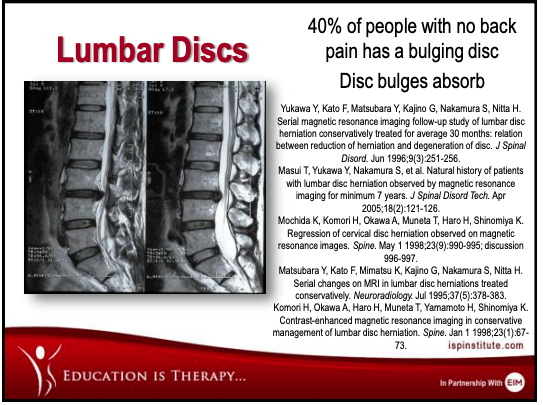
(Infographic Courtesy of the International Pain and Spine Institute)
Or taken to an even more peculiar end, those who experience phantom limb pain.
Pain experienced in a limb that is anatomically no longer present, as in the case of amputee individuals.4
Is their pain experience just made up and in their head?
The tenants of the current medical model would surely dismiss this experience as one that does not fit the criterion of tissue pathology and thus delegitimize the phenomenon and perhaps explain it as a purely psychological dysfunction.
The Body-Mind Split and How it Misguides Pain Relief
This body-mind split is flawed and has its roots once again in cartesian philosophy.
Following the Renaissance period, scientific efforts focused on increasing their understanding of the neurophysiology of the nervous system.
Pain was seen as an overstimulation of various receptors in the body.
With the focus on nerve fibers, Gate Control Theory remains arguably the central theory to explain the pain experience.
Melzack and Wall proposed that a gating mechanism exists in the dorsal horn of the spinal cord.
Small nerve fibers they called “pain receptors” and large nerve fibers, “normal receptors” synapse on projection cells, which travel up to the spinothalamic tract to the brain and inhibitory interneurons within the dorsal horn.4
This interplay was thought to determine when a “painful” message would proceed to the brain.
Although Gate Theory explains many observations regarding pain, it has shortcomings in light of the newer research on pain.
Gate Control cannot account for phantom limb pain.
It cannot explain pain below the level of injury in complete spinal cord injury.
It cannot account for the complex immune and inflammatory processes which have now been shown to be key components to pain.
It cannot explain emotional issues pertaining to the pain experience.
And finally – it does not account for various social aspects of pain.
Is Tissue Damage the Cause of Lower Back Pain and Pain in General?
Tissue healing is only part of the puzzle when it comes to healing from pain.
It is certainly not the only cause of lower back pain.
If clinicians are to help patients through pain and more broadly on an epidemiological level, solve the opioid crisis (the pharmaceutical solution to chronic pain) – we need to reevaluate the outdated models of pain.
Only then will we be able to find holistic solutions to fixing back pain
I am certainly not the first to write about shifting the pain paradigm and I have many to credit for bringing this information into the light.
I would again like to formally acknowledge Adriaan Louw, Emilio Puentedura, Stephen Schmidt, and Kory Zimney.
With the latest research shedding light on the neuro-complexity of pain and its associations, I will leave you with a relatable example and a few final points.
Pain and Why Gate Theory Can’t Explain It All
Let’s say you are walking and sprain your ankle.
It would likely result in pain.
Based on gate control and neurophysiology it would be easy to describe the process in the following way:
The tissue damage stimulates A-delta and C nerve fibers that send “pain messages” via sensory afferent nerves to the dorsal horn of the spinal cord.
The “pain messages” are passed from the dorsal horn via second-order neurons to the brain to call upon action!
For example – seeking medical help, canceling weekend plans etc.
Now take a similar but slightly different situation:
You are walking across the street and sprain your ankle and out of the corner of your eye you see a speeding car headed your way.
What do you do?
Of course, you get out of the way and make your way to the other side of the street paying minimal attention to the sensation of your ankle.
It is not until you reach the other side of the street and are in relative safety that the ankle begins to throb with pain.
How did this happen?
If the injured tissues in the ankle had sent “pain messages” to your brain in the middle of the street, the pain could have been so debilitating that you fell on the floor grabbing your ankle and subsequently got run over by the car.
The only thing your ankle did in the moment was send a danger signal to your brain but your brain made the objective decision that getting run over by a car is probably worse than the tissue damage received by your ankle
And so, you decided to get the heck out of the way and cross the street.
The ankle contains nociceptors that are easily activated by inflammatory chemicals, temperature changes and mechanical input from the tissues.
The message will be passed to the spinal cord and then the brain via second order neurons.
Finally, the pain is “felt” as a construct of the brain.5
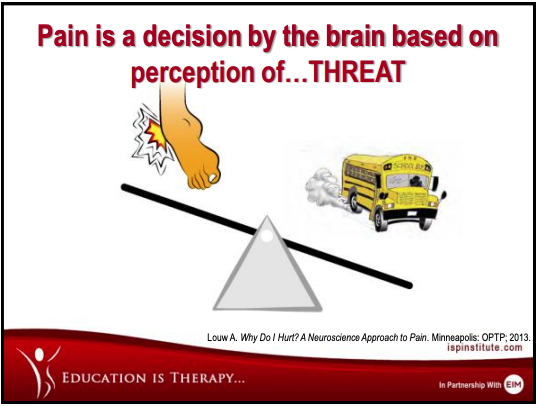
(Infographic Courtesy of the International Pain and Spine Institute)
Pain and The Brain
Pain is a decision by the brain based on perception of threat.6
Pain is a brain construct.
The brain constantly receives information from the environment, as well as the body to determine the most appropriate response based on survival, experience and threat.
As mentioned, many people experience pain despite a lack of tissue damage.
Perhaps then we must reevaluate pain and begin to construct an evaluation based on socio-cultural and psychological factors.
Much like the ear contains various vibrations and sound receptors, messages from these receptors are processed into “hearing” by the brain.
The eyes contain light receptors and send messages to the brain which are translated to produce “vision.”
Muscles, tendons, ligaments, joints and skin all contain receptors – nociceptors.
Not “pain receptors” that the brain processes into the experience of “pain.”
It is important to make this distinction as the body does not contain pain receptors, it contains receptors responsible for transmitting electrical signals.5
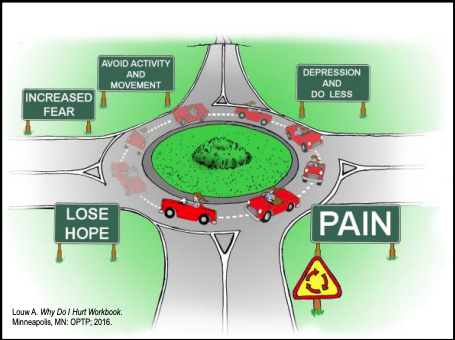
(Infographic Courtesy of Adriaan Louw in the Why Do I Hurt Workbook)
How It Relates to Your Lumbar Backache
The brain, through the aforementioned points, evaluates these signals and responds in a unique way based on the individual circumstances at hand which are a blend of physiological processes, context, mental state and social reality.
In short, the experience of pain is a blend of input mechanisms, output mechanisms and processing mechanisms.
The greatest thing that we as clinicians can do is listen to our patients’ experience of pain, their beliefs about their pain and figure out a treatment plan that encompasses the biopsychosocial tenants.
Only then will we be better equipped to solve the mystery of chronic pain which has haunted strict Cartesian subservients for centuries.
The cause of your lumbar backache is in the brain, not just the lumbar spine itself!
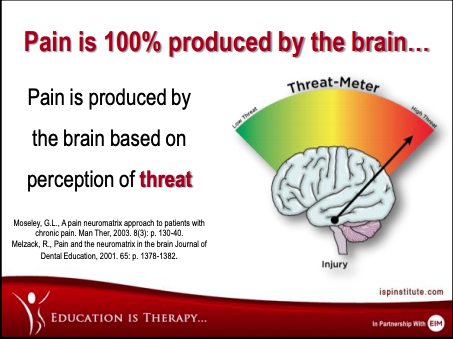
(Infographic Courtesy of the International Pain and Spine Institute)
Lower Back Pain Stretches and Getting Rid of Lower Back Pain
Now that you understand pain, it is time to apply this new found knowledge to fixing your lower back pain in the form of stretches and stability exercises.
Although lower back pain can feel like a life sentence, relief is in close reach.
Assuming that you have been to a doctor already and they have cleared you for physical therapy, we can begin implementing some strategies that will get you on the right track to solving your lower back pain.
If you have not had any success with the exercises that you have been using to relieve your back pain, it is time to try something new.
I didn’t want to overload this page with too much content, so you can begin by implementing these stretches in this article I wrote.
You will find in depth explanations and videos to guide you.
Then if you want to take it a step further, keep reading below.
Back Exercises for Lower Back Pain
I have had a lot of success getting my clients out of pain by implementing a few foundational exercises for their back pain.
These are the same foundational exercises that I start with FIRST after I assess my clients needs.
Although I am not there with you in person to prescribe modalities for your exact needs, these foundational exercises are gentle and highly effective.
After years of implementing them with my clients and my own personal back pain, I believe that these should go in your tool belt as the foundation of your primary strategy.
You can download a free guide with my top three how to fix back pain stability drills here.
The guide comes with explanations and videos of how to perform each exercise properly.
As mentioned above, I have also written another article here about the best stretches for lower back pain which also includes explanations and videos to get you started.
I would also be more than happy to help you on an individual level if you want to reach out directly here.
References
1.) Global Burden of Disease Study C. Global, regional, and national incidence. Prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. Aug 22 2015;386(9995):743-800
2.) Merskey H, Bogduk N. Classification of Chronic Pain. 2nd ed. Seattle: IASP Press; 1994
3.) Chen J. History of pain theories. Neuroscience bulletin. 2011;27(5):343-350
4.) Melzack R. From the gate to the neuromatrix. Pain. 1999;Suppl 6:S121-126
5.) Louw Adriaan et al. Pain Neuroscience Education, Teaching People About Pain.20186.) Moseley GL. A pain neuromatrix approach to patients with chronic pain. Man Ther. 2003;8(3):130-140.
Who is Jakob Roze?
Jakob Roze is a Strength and Conditioning Coach and founder of RozeFit. His practice centers around empathic communication and relationship building. With an emphasis on pain-free, functional movement patterns and strength training, Jakob Roze assesses each individual’s needs and prescribes exercise modalities appropriately in order to facilitate long term gains in strength and health. He draws from evidence based approaches and applies the knowledge in a personalized fashion to facilitate body and lifestyle transformation amongst his clients.


