So this year, I have been absolutely obsessed with lipidology.
I thought I had a basic understanding of the atherosclerotic disease process, but it wasn’t until I came across the work of world-renowned lipidologists like Tom Dayspring, Allan Sniderman, and Herbert Stary that I truly realized how small my knowledge base truly was.
Their work has inspired me to learn more about the disease process because of how significantly it affects the world’s population.
After all, cardiovascular disease is the leading cause of death worldwide!
It deserves some airtime, and unfortunately, we all too often overlook this disease because of its relatively silent manifestation until it is too late.
My previous article discusses how cardiovascular disease begins in infancy and progresses throughout your lifetime.
In this article, I want to take a closer look at the evidence for this unbelievable fact that the beginning stages of cardiovascular disease are present during the first decade of life.
But First, Brief Overview – What Is Cardiovascular Disease?
For the sake of an introduction, I want to give a brief summation of what cardiovascular disease is in the first place.
Something easy to understand before we get into the weeds a little.
The bottom line is this.
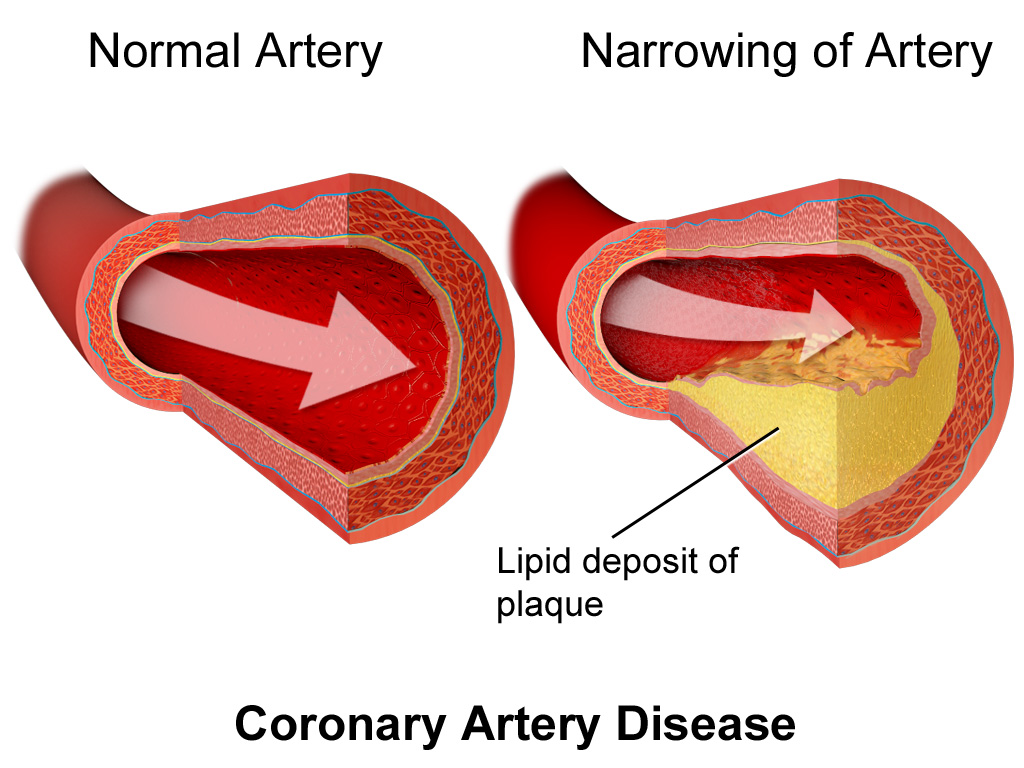
Cardiovascular disease is a complex pathology of the heart and its associated vasculature.
More specifically, cardiovascular disease often refers to atherosclerosis which is a disease of the arteries characterized by plaque deposition on their inner walls.
Ultimately, at the root of the atherosclerotic disease process is the formation of plaque from lipid accumulation.
This lipid accumulation comes from a lipoprotein called the low density lipoprotein.
Quick aside, you need these lipoproteins to carry lipids in your plasma because lipids are hydrophobic, meaning that they don’t mix with water.
And since your plasma is mostly water, you need a transport vehicle for those lipids.
But the problem is, these LDL particles often end up in the arterial wall where they should not be and then they become oxidized as you will learn about in the next section.
The bottom line is that you can’t have atherosclerotic disease without the presence of LDL particles, full stop.
LDL Particle & LDL Oxidation
These LDL particles need to be oxidized to catalyze the formation of what are known as foam cells.
Foam cells form when a macrophage comes along and scavanges the oxidized LDL particle.
These macrophage foam cells then become the spark for an entire inflammatory cascade which ultimately results in the next step of the process.
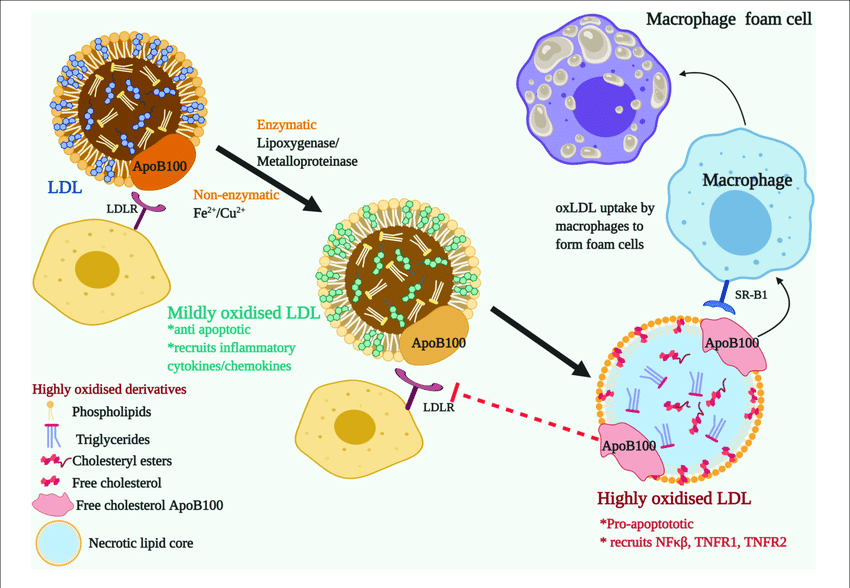
The Inflammatory Cascade
The foam cells get bigger and trigger an inflammatory response by the immune system in an attempt to repair the damage.
The problem is, this immune response in an attempt to repair the damage actually ends up creating more damage.
Chemical signals then trigger smooth muscle cells which are transformed into secretory cells that lay down a matrix to heal the artery wall.
This matrix ultimately becomes the fibrous cap of the atherosclerotic plaque!
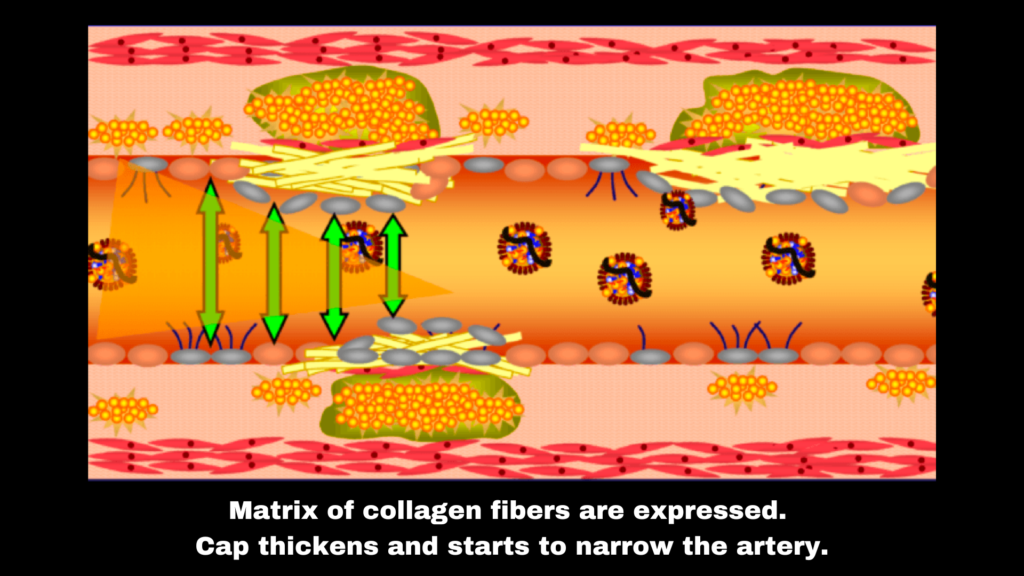
That is, the abnormal growth within the artery wall which ultimately causes the artery wall to get smaller.
The lesion in its most advanced stage eventually becomes thrombotic or in other words, breaks off in the form of a clot that ultimately clogs the vessel, causing the heart tissue or other organs to become damaged.
This final event is also known as a heart attack or a stroke.
The Silent Killer
There is a reason that heart disease is called the silent killer.
The disease process is progressive and there are often very few associated symptoms until the disease reaches its advanced stages.
Let’s take a look back in time though and examine where, why, and when this first assault on the arterial wall begins to take place.
It’s much earlier than you would expect.
The Initial Lesion: Type 1
Herbert Stary and colleagues published a wonderful paper titled A definition of Initial, Fatty Streak, and Intermediate Lesions of Atherosclerosis.
This paper examines the histology of atherosclerotic lesions and their associated pathologies.
Note that since this paper was written the classification has changed a bit but the underlying concepts are still just as relevant.
They begin by discussing the Type 1 lesion, which represents the very initial changes that are recognized in the arterial intima.
These lesions consist of the first detectable quantities of lipid deposits in the intima and the cell reactions associated with such deposits.
You can see in this picture which displays small, isolated groups of macrophages consisting of lipids droplets.
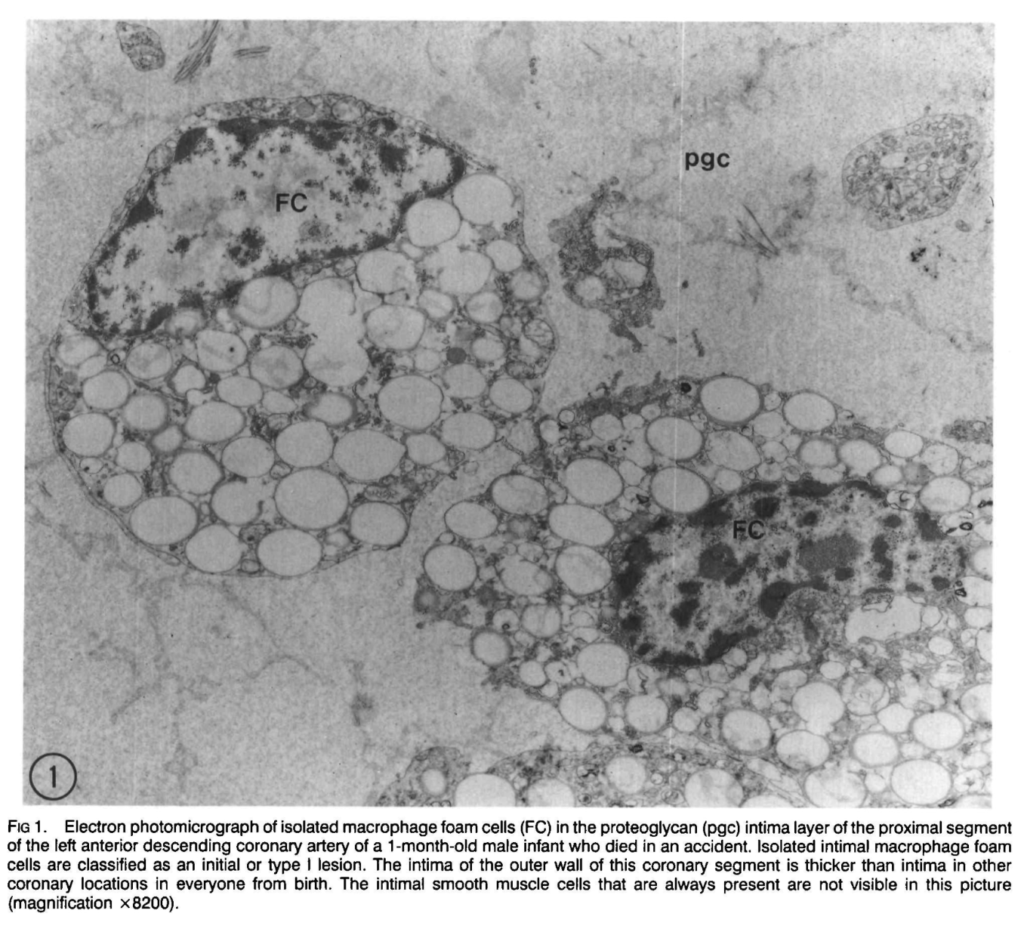
These are also known as foam cells.
A crazy fact is that in the first eight months of life, 45% of infants have macrophage foam cells in their coronary arteries!
Gives you a sense of when this whole heart disease process starts.
Now I’m certainly not claiming that the majority of babies have the clinical manifestation of cardiovascular disease.
The point I’m trying to make is just how long ago the initial stages of the disease start.
These macrophage foam cells are in essence, the blueprint by which the atherosclerotic disease process builds its foundation upon.
And going back to my point before about how LDL particles are necessary for this disease process.
Stary states in his paper that “chemical and immunochemical data indicate that the initial intimal macrophage foam cells are both a sequel to and a cellular marker of pathological accumulations of atherogenic lipoproteins.”
In other words, those LDL particles are the source of this entire cascading storm which is about to begin in the artery wall.
Progressing to the Type 2 Lesion
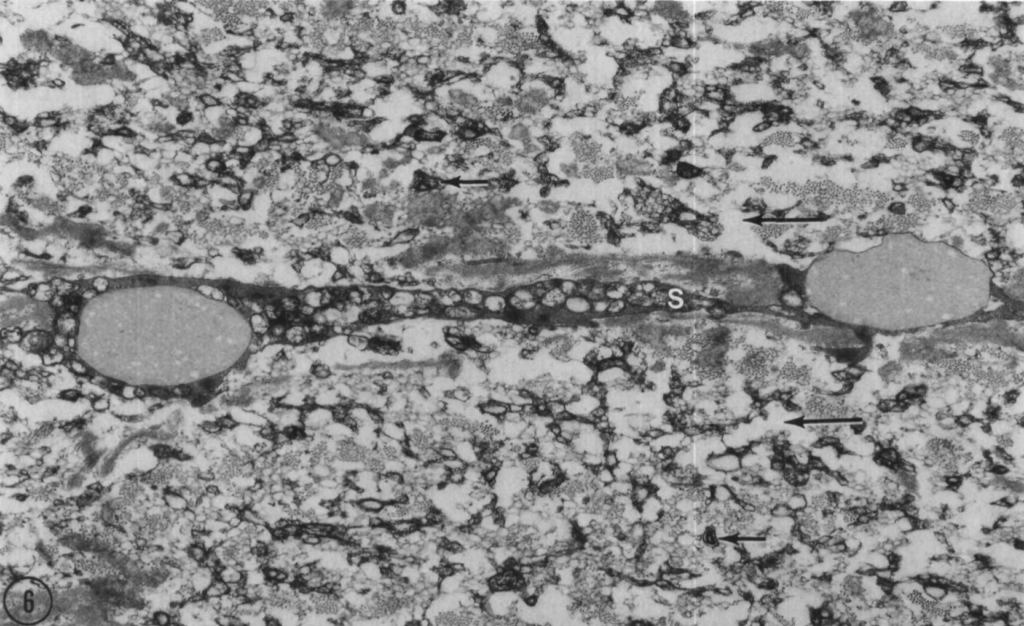
The type 2 lesion is characteristically defined by the presence of a fatty streak.
This fatty streak is visible as a yellow-colored streak, patch, or spot on the intimal surface of the arteries.
At this point, the lesion also contains lipid droplets in addition to the macrophages.
Type 2 lesions don’t present with symptoms and are still considered to be in the early stage of atherosclerotic disease development.

Interestingly, most adolescents have evidence of fatty streaks in their aortas.
You can see in the photo above which displays the initial thickening of the inner layer of the artery (i.e. intima).
Taking a pause for a moment, it is important to address the driving cause behind lesion progression.
While the mechanisms are numerous and complex, one thing remains consistent.
The LDL particle.
To quote Stary regarding the progression of the Type 2 Lesion:
“The mechanical forces in locations in which type 2 lesions are susceptible to progression cause an increased influx and early accumulation of lipids in persons whose whole plasma lipoproteins exceed certain thresholds.” One of these forces, low shear stress, increases the time of interaction between blood borne particles (LDL) and the arterial wall.”
We come back once again to the unambiguous fact that the cholesterol-rich lipoprotein (LDL) and its interaction with the arterial wall are the necessary but not sufficient requisites for the development of atherosclerosis.
I say this as a prelude to the strategies which are preventative when it comes to heart disease.
Getting rid of that that LDL particle and preventing it from entering the artery wall are critical components to avoiding injury to this precious tissue.
Lesion Type 3 & 4
Lesion Type 3 is considered the intermediate lesion.
It is not yet advanced by histological classification but bears the presence of extracellular lipid droplets that have pooled.
You can see in the photo below, the little black arrows show where the lipid droplets have pooled.
The photo is a super magnified electron photomicrograph of the proximal anterior descending coronary artery from a 29-year-old man who died in an accident.
After its intermediate state, the lesion has progressed to Type 4 to become advanced by classification standards.
Type 4 lesions are defined by their lipid core, intimal disorganization, and arterial deformity.
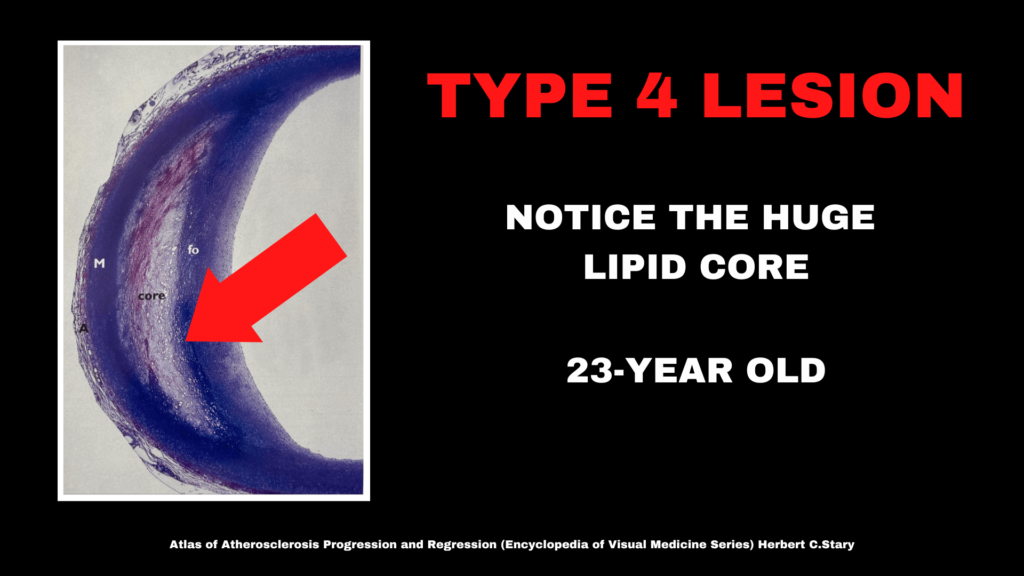
These types of lesions are most apparent by the third decade of life.
But you can see in the photo above that this individual was only 23-years old!
Again, emphasizing the point that the initial stages of atherosclerosis begin well before middle-age.
I’ve written more about the advanced lesions in the article if you want to read more.
Lesion Type 5 & 6
The lesion has developed a defined lipid core with fibrotic layers and is calcific by its morphology.
Eventually, the surface of the lesion becomes vulnerable to defects and the plaque could rupture, causing a thrombotic event.
AKA, a blood clot and subsequent cardiac event.
The sad thing is, although these lesions are considered advanced by their morphology, they do not always present with overt symptoms.
Many people die suddenly.
Why You Should Care

All this is to say that, ultimately, you should really care about this process.
Not so much for the sake of understanding its complexity but rather that whether you want to admit it or not – atherosclerosis affects you throughout your life.
You may not be symptomatic, but the reality is – all of us experience the disease process to some degree.
What matters is how much the disease progresses, which is precisely why it is imperative to stay on top of your preventative measures.
If you are middle-aged and your doctor told you that you have high cholesterol, high blood pressure, high blood sugar, or any of the other risk factors for heart disease, it’s time you begin taking action.
These risk factors significantly increase the probability that you will have a cardiac event in your lifetime, and if your goal is to stick around as long as possible to show up for your loved ones and family, it warrants taking action.
The great thing is that there is so much you can do to reduce your risk for cardiovascular disease.
And the best part is that most of the strategies are free and easy to implement.
Exercise is probably the best tool we have aside from pharmacological interventions.
I have written at length about these strategies, which you can read more about here.
I’ve dedicated my entire career to helping middle-aged individuals reduce their risk factors by improving their metabolic health through diet and exercise.
You might be interested in some more guidance, in which case you can learn more about my coaching opportunities.
As always, feel free to reach out with any questions you have, and I would be more than happy to get you started!
Cheers.